Health Issues
This page provides details about my experiences with urinary tract infections and kidney stones, pressure sores, hospitals, and medical updates.
Urinary Tract Infections and Kidney Stones
Antibiotics: These two items are the bane of spinal cord injury victims – at least for me. Initially I had a couple of infections a year, which were easily treatable. The frequency of infection increased as I aged. My doctors at the time simply prescribed another course of antibiotics. In fairness, I too participated in that treatment program because I wanted the symptoms to go away and to get on with my life. These actions ultimately proved to have serious consequences.
Around 2002, I developed significant symptoms that required hospitalization. I had extensive kidney stones and a drug-resistant Pseudomonas bacteria. Numerous procedures, surgeries and IV-delivered antibiotics in the hospital, as well as treatments at home for months after, put the bug back into a box. However, it was never eliminated. Instead it colonized in my body. When this occurs, the bug isn’t active enough to make you feel sick. I just became less active and had other ill-defined symptoms, but I was surviving, more or less.
Sound waves: From 2002 though 2005 I visited the lithotripsy center numerous times to blast my kidney stones with sound waves. But this had little lasting effect. As soon as one stone was gone, two more replaced it.
More Antibiotics: In early December 2006, I again became very ill. When my fever passed 104º and I was unable to transfer from my bed, I called 911 and enjoyed a ride in an ambulance to Adventist Hinsdale Hospital. I might mention that the transfer to Hinsdale Hospital was a new experience as United Healthcare had recently bought my insurance company (the insurance that costs over $1,000 a month with $50-$750 co-pays). They had been in a pissing match with Advocate Hospitals, so I had to find new doctors and hospitals. Anyway, the new doctors at Hinsdale decided that all I had was a simple bacterial infection (despite my telling them my complete history – in writing) because the urine culture only showed a simple E. coli infection. After two days of IV antibiotics, I felt much better. They decided I could go home with an oral antibiotic.
Stent: After being home for about a week and finishing the antibiotics, I started to decline again. The oral antibiotic was resumed, and a urine sample taken to culture. Christmas night my fever soared to 105º. I again dialed 911. The Tri-State Paramedics responded almost before I could take my next breath and transported me to Adventist La Grange Memorial Hospital (another new hospital). The results of the culture showed my good friend Pseudomonasaeruginosa was in control. I was admitted into a regular room. Within a few hours of admission, my blood pressure took a precipitous fall. I remember readings of about 60 over 40. They say that’s not too good. Near panic (at least how panic manifests itself in a hospital) set in. A bunch of nurses and doctors (5-8) from the intensive care unit were all very busy; they wouldn’t transport me due to the crisis.
My single IV line failed, and no new veins volunteered for IV duty, so a surgeon (I remember that his name was Zawacki) was summoned to my room to install a central catheter. After it was installed, they started pumping huge volumes of fluids into me. Fancy drugs were administered to help raise my blood pressure. The drug use required almost full-time babysitting, but after a while, I began to respond. In a few days I was on the road to recovery. I looked like “Marshmallow Man” from the fluids. I had almost no strength. I had gone into septic shock, which was likely due to a blockage in my right kidney caused by the stones. This blockage resulted in bacteria making its way into my bloodstream. To temporarily correct that problem, they inserted a stent into my right kidney. After many months and two surgeries, including more rounds of IV antibiotics, I recovered, more or less – with a little more emphasis on the less. When United Healthcare and Adventist terminated their contract, I was forced to find another new set of doctors. This couldn’t have happened at a worse time. At termination I had stones in only one kidney. The delay caused by the dispute, plus scheduling delays at the new hospital (Loyola), resulted in more kidney stones forming in both kidneys.
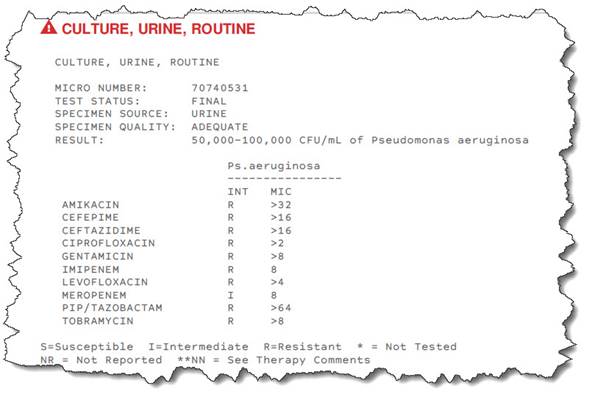
Surgeries: I think my single surgery at Loyola was successful; however, I wouldn’t let Loyola treat my fish because of their careless charting/record keeping and arrogant doctors, including know-it-all second-year residents. (There may be exceptions in other practice areas.) For example, they charted that I was diabetic and that my blood pressure was 195 over 100 despite the fact that it was never recorded anywhere near that level. It took significant effort to get these issues resolved. When errors like these occur, your life could be at risk. Fortunately after several months, United Healthcare and Adventist kissed and made up, so I gladly went back to Adventist. My next visit to the lithotripsy center was in late March 2008. After extensive analysis of my urine over several days, they determined that I was making too much of a particular chemical substance. They placed me on a medicine designed to change my urine’s chemistry. It seems to have done the trick because I did not make new stones for six months. However, as of June 2008, the bug continued to develop resistance. A culture showed a resistance to Cefapime and Ceftazadime, although a subsequent culture taken within several days did not. Assuming the worst, this left me with only two effective IV antibiotics. My view of the situation was somewhat grim. I was scheduled to have both my kidneys operated on to flush the remaining stone debris from them. This debris was thought to be infected with the resistant bacteria. After these hiding places were removed, treating the bug should require the remaining antibiotics to cure me. Although I’m a skeptic, I became hopeful.
In September 2008, having been on IV antibiotics essentially non-stop for about six months, I had surgery on both kidneys to retrieve kidney stones. The surgery was judged successful based on the operating report. However, it left many, many stone fragments behind that had settled into the lower lobes of both kidneys. Further, the bacteria was still present in the cultures. I asked the doctor what else beside IV antibiotics we could do. Several therapies were suggested.
Intravescular Irrigation: This therapy injects 60cc of a dilute mixture of an antibiotic into my bladder twice a day. Intravascular irrigation is a nice name for this procedure, which requires catheterization and then injection of the medicine using the catheter.
Methenamine Hippurate: The next therapy is even more interesting. The doctor suggested Methenamine Hippurate to combat the increasingly drug-resistant bacteria. This medicine is a time-released variant of Mendelamine, which I had asked different doctors about using on a number of occasions, and they had decided that it wouldn’t help. In the urinary tract Methenamine Hippurate turns into a diluted concentration of formaldehyde. After more than 45 days with no IV antibiotics and no PICC line, my last urine culture didn’t have any nitrates, white cells or bacteria detected. This is remarkable considering my recent history. The skeptic in me was right; additional urine cultures confirmed that the bacteria was still present. In retrospect, I believe that the negative culture was a false negative. It simply wasn’t given sufficient time as the clean report occurred after only two days. All other cultures took three, four or even five days before the final report was issued. Anyway the infectious disease doctor determined that my symptoms didn’t warrant IV antibiotic treatment. Withholding treatment has lead to a journey that I think is worth recording.
Lots of Fluids: Bacteria can “colonize” in their host. This means that the bacteria are living in me but not causing significant symptoms. Between October and early December 2008, my temperature remained in my normal range of 96 to 97º Fahrenheit (I use Braun ThermoScan). At that time I felt OK, but not great. Then in early December I voided (see inversion) a significant number of stone fragments left over from the September surgery. Almost immediately I took a turn for the worse. My temperature at times “spiked” to 99.5º (remember, this is more than two degrees higher than my normal). I suffered from malaise and was always cold. So cold in fact, I wasn’t comfortable in a room at 76º wearing two heavy sweatshirts. Despite these symptoms the doctor didn’t think they were significant enough to offset the risks of treatment. To say that I “freaked out” would be an understatement. Another round of IV antibiotics with one of the remaining drugs and another hospitalization were almost more than I could handle. In response and to feel that I had some degree of control, I began drinking 150 to 180 ounces of water, cranberry juice and other fluids daily. I increased my dosage of Menthenamine to one gram three or four times a day, depending on how much debris I saw in my urine and how I felt. I became obsessed with taking my temperature. These steps (at least the first two) seemed to make an improvement. However, there were days when it was all I could do to simply exist. Mostly I was in bed. Usually in the mornings I felt better, and I could be more active. This phase continued more or less in a predictable fashion. If I kept my activity level low enough, I was pretty stable; if I increased my activity, my condition worsened the following day. It was during these worse periods that I began to notice increased debris believed to be mucus floating in my urine. It looks like little wispy white clouds and can be seen with the unaided eye; white cells can’t be seen, but a milky appearance to the urine may be noticed. My urologist said that in my case they were not significant. Perhaps they weren’t, but they seemed to be related to my activity level, fluid intake, medicine dose and not feeling well. I guess I will never really know. Around the middle of February my temperature trended down to my “normal” range. I felt better, was able to live at a more comfortable room temperature and became a bit more optimistic.
A couple of significant points:
Too much water intake can result in low potassium and/or low sodium in your blood, either of which can pose a potentially life threatening condition. My blood work indicates my levels are OK. I informed the doctor (albeit after the fact) of my increased dosage of Methenamine. The urologist was OK with my decision and increased my dosage. Incidentally I did consult medical references prior to increasing the dosage. I believe I was well within the guidelines. As an aside a number of years after I first had the resistant bacteria, I had a phase where the bacteria colonized with minimal significant symptoms. That journey included periods of vertigo during the transition from IV treatment but resulted in my remaining off antibiotics for about two years. That period continued until invasive surgery, which resulted in the months-long treatment. I am hopeful this may mark such a period!
March 2011 update. Concerning my colonized bacteria – March hasn’t been a great month, first I became symptomatic with symptoms consistent with an bacterial infection and entered the hospital. Early treatment pending the laboratory results consisted of IV antibiotics. By the 2nd day it was known I was septic (infection in the blood) although I was stable except for a high temperature. By March 3 the bacteria was identified as E. Coli that had mild antibiotic resistance and my antibiotic was changed to Ertapenem. The doctors recommended removing the remaining kidney stones in my left kidney while continuing with the antibiotics. I was discharged to home with continuing IV therapy. The surgery was quickly scheduled and was performed on March 14, 2011. The surgery was deemed (by the doctors) successful and I was discharged on March 17, 2011. The belief is I have no stones, hence no place for the bacteria to hide from the antibiotics so this may be a new chapter in my life and I am hopeful!
April 2011 update. It seems that my optimism in March was doomed to be dispelled. A later urine culture showed the P. areginosa remains. Further my doctors shifted their position on possible paces for colonization and my daily medicines. In part I believe they are operating on incomplete and/or misinformation (part of the medical communities of specialization with multiple doctors involved) at least as far as I am able to recall or verify. Accordingly I wrote the letter you can read read the letter here June 2013.
Having found the courage to offer myself up to the gristmill, starting with a round of doctor visits and tests in May, I was scheduled for surgery on June 10th. This procedure was to Bi-lateral Percutaneous Nephrostomy with Cystoscopy. This two-step surgery required Interventional radiology to insert guide wires through my back into both kidneys then the surgeon uses them as a road map. Sadly, after the guide wires were inserted and while waiting for the perc-neph, I developed a significant fever accompanied with chills and rigor. Here we go again with sepsis. The perc-neph was canceled and I was admitted to the hospital to treat the sepsis. The assumption being made that the bacteria P.ariginosa had gotten into my blood, so specific antibiotics were ordered for treating that bug. The blood cultures take several days to complete and they revealed that I had a rather run of the mill enterococcus (Not vancomycin-resistant enterococci (VRE) which I have had in the past) and my antibiotics were adjusted according. While this bug was rather plain-jane from the perspective of antibiotic susceptibility and treatable with a wide range of antibiotics, the bug once in the blood does have a fondness for attacking heart valves, this makes the disease Infective Endocarditis a concern as left untreated you simply die. Between my regular physician, the infectious disease doctor and my urologist they carefully assessed my symptoms and found that I did not have the signs of that disease. Therefor they would be watchful for any new symptoms before further tests or treatment and this was noted in my chart.
June 17 2013. The second part of the surgery was completed and the urologist reported he removed something like 40 to 50 small stones and several stones in the 4-6 millimeter range. My surgeon was confident that all the stones were removed except for one that he couldn’t reach due to the placement of the guide wires or limitation of the instruments. It was possible that object was a calcification and was not in the “machinery” of the kidney and therefore may not be a concern. Stents were inserted into both of my ureters. Now having been in the hospital for 8 days I was suffering gastro problems which is normal for me and the only effective solution is to get me out there and return to my normal routines at home. The surgery had taken a long time and it wasn’t until about 7pm that I was back in my room. I was still suffering from the effects of anesthesia and the surgery. Not having my routine medicine, food or water for about 24 hours my guts were a mess. About 9 pm, just when I was feeling up to eating and drinking a little, my nurse breezed in and told me my stand-in doctor had ordered no food or drink (I was dying of thirst) as she had scheduled an invasive test with anesthesia for the next morning. She thought I might have endocarditis. I objected but apparently too weakly as I was still suffering from the day’s activities.
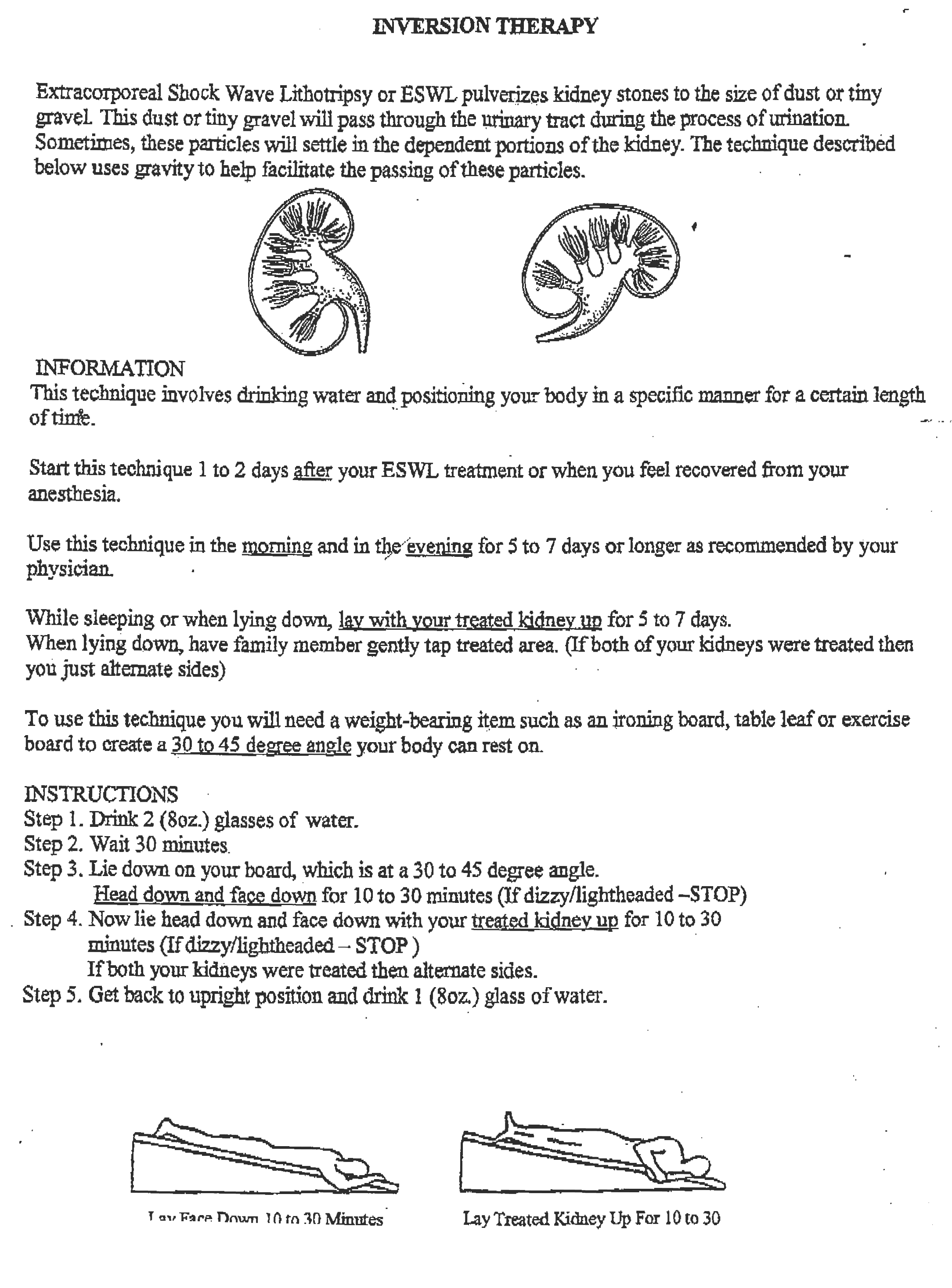
About midnight I was feeling up to the challenging these orders, writing to all my real doctors (having a notebook is a benefit) and created quite a fuss. Its turns out that stand-in doctor had ordered this test because she miss-read a single blood test as two separate positive tests for the bacteria enterococcus in the blood – a serious mistake. One of indicators to suspect endocarditis is two consecutive positive blood tests. It was this mistake coupled with her incomplete reading of my chart that had caused her to order the test. As a rule, I simply don’t take kindly to ANY doctor making orders that affect my well-being without speaking with me, especially when the procedure is invasive. The next morning I had confirmation from my other doctors that endocarditis while a risk was not yet suspected in me and that the stand-in doctor had acted prematurely. I had a very direct meeting with her – OK really a confrontation as I was and remain pissed with her. The result of the meeting was I essentially removed her from my care. I have heard she was upset by my directness however, she was defensive and when it comes to my health and treatment, I simply won’t tolerate it. Had she been upfront with me we might have resolved this matter more amicably. July 15, 2013. Are we done yet? Sadly, no, a follow-up X-ray and CT scan revealed what looked like two or three more stones with both kidneys affected. Had another surgery on July 15th. It was successful and they removed another 25 or so little stones. The CT saw these stones as only 2 or 3 so the surgery expanded to accommodate. This surprise is not uncommon as the CT resolution while much better than X-Ray still is lacking ability to see small tightly packed stones and they often appear as a single stone) This meant instead of a quick 45-minute surgery, it became a little longer lasting about 4 hours. Essentially I had begged the surgeon to perform this surgery on guts with no anesthesia or sedatives and I felt good following it going home by 3:30 pm. Continued on the IV antibiotics until July 19th. The theory all along is if they can get me completely stone free, there is a chance that the multiple drug resistant bug will not be able to survive the antibiotics that are still effective against the bug. As of July 24th, the laboratory hasn’t been able to detect the bug and this is a positive development. The stents were removed on July 30th during an office visit and so now, life is good… Inversion Therapy: After my last surgery, inversion therapy was suggested to help rid me of stone fragments. The idea is to elevate the body (head down) at a 35 degree angle, which better positions your kidneys so that stones that accumulated into the lower lobes can travel to the ureters and then exit the body. I was given instructions to prop an ironing board at the appropriate angle and somehow position myself on the ironing board. I doubt that even an able-bodied person could do that task safely. My solution was to purchase a small electric hoist, bolted through the floor with a pulley attached to the ceiling, which then is attached to a lifting strap affixed to the bed. The Chicago Electric Model 44006 hoist is relatively inexpensive and is available from a variety of sources. It is a self-contained unit, runs on normal household electricity and plugs into a standard outlet. For the ceiling attachment I used two heavy-duty screw eye hooks each rated at 350 lb. I then inserted a steel bar between the hooks. The purpose of two eye hooks was to distribute the load and to allow better alignment of the pulley than the ceiling rafters allowed (the hooks must screw into the rafters). In use the load is likely less than 150 pounds as the much of the weight is still supported by the bed. The hoist’s hook is attached to a nylon lifting strap. It loops twice around the mattress, box spring and bed frame as this cinches and keeps the items all together when in use. I am pleased to report that almost immediately I was rewarded by voiding some stones. After a few days of treatment, a total of 15-20 small kidney stones and/or stone fragments were flushed from my system. After I made my design, it occurred to me that I could have put a sheet of 3/4″ plywood between the box spring and bed frame to avoid bolting the hoist to the floor; cut the plywood the width of the bed and long enough so that wood protrudes at the foot and allows the hoist to be attached. This solution would need couple of ratcheting cargo straps to strap the mattress, box spring and bed frame together.
I caution anyone who attempts my solution that they do so at their own risk!
1-31-2015 Routine CT Scan needed for upcoming visit to the urologist performed at 7 AM. A few hours later and Surgeon calls about 11:45am. Can’t be good suggests we meet in ER. Partial obstruction caused by stone .75 X .5. Emergency surgery at 3pm. Despite failure in the past with help from interventional radiology stents placed successfully in place both sides. No anesthesia at my request and I think the anesthesiologist was crushed – at first, he wouldn’t believe it, but the surgeon confirmed it would be okay. Have elevated white cell count, because of my history IV started with Zosyn. Bugs were identified Pseudomonas aeruginosa (my old friend antibiotic resistant critter) and an antibiotic friendly Enterococcus group d decision was made to remain on Zosyn with a PICC line. Discharge when white cells fall – achieved Tuesday. Discharge process simply a goat rodeo no action discernable 12 hours later Wednesday, stir up some folks. Social worker doesn’t have a clue, tells me I must have IV pump and only 3X a day – wrong. Call IV pharmacy to straighten out. Discharged Wednesday afternoon with IV at home via (old news) PICC. Discharge process is slower than the flow of molasses at 33F, takes an assertive person to stir up the pot. Despite the pushing from my end all 3 docs all managed to get in one final visit that will raise my tab $50 a pop just so they could say goodbye – nothing else accomplished. Heartwarming to me to say the least! Will return to hospital on 2//12/2015 for more surgery, a day or two in the hospital and if all goes well discharge with IV at home for a week or so and then resume my life.
2-12-2015 Bilateral Percutaneous nephrolithotomy retrograde ureteroscopy with laser. Surgery was scheduled to begin at 2pm, however delay after delay occurred and the surgery didn’t start until 6:20pm. It was completed around midnight. I requested no anesthesia (I think this is the 4th time I have had surgery without anesthesia) and the surgeon allowed. This time he left the video monitor in a position where I could view the entire procedure and it’s simply amazing. The laser (used to break up large stone) when firing makes a rapid clicking noise, the light is non-visible but damaging to the eye and you need special eye protection. Could feel a physical sensation mirroring the clicking sound in my neck and/or back of head – it’s a hard sensation to describe and was a bizarre feeling bordering on a mildly uncomfortable or at least a disconcerting sensation. The closest I can’t relate it’s like a chisel and hammer and it carves / explodes the stone into smaller chunks that can then be withdrawn though some rather small spaces. The laser causes a vaporization bubble and this action then causes cavitation and that is what breaks up the stone. I had 4 large stones requiring the laser and hundreds of smaller stones that were irrigated or basketed out. I was admitted to an observation room around 1am and only got a few hours of sleep. Discharged around 11am Friday. Overall feel ok though a bit tired. Still on the IV 4 times a day and that’s a drag.
4-29-2015 Dr. Fredric Coe’s report: 60-year-old man with kidney stones. First stone was 10 years ago. Last episode was yesterday. In between he has had hundreds of stones. Stones are made of CaP 2/12/15 analysis shows hydroxy and carbonate apatite. No quantification, this is a kind of summary from the laboratory. He has had 6 or 7 Shock wave lithotripsies; 4 PERC- Nephs perhaps bilateral; URS 4 times as well. Chlorthalidone 25 mg 2 times daily + potassium citrate 10 mEq 3 daily. The citrate is for 10 years, the CTD for 4 years. These meds did not do any good for his stones, perhaps worsened them. The citrate appears to have had no effect. The last 5 years have been an accelerating trend. He is infected with pseudomonas + enterococcus. I have two urine studies from 12/16 and 12/17/14. Both show marked hypercalciuria with high pH he takes K citrate and SS CaP 1.63 and 2.03. This is on CTD 50 mg/day! And a modest urine Na excretion 104 and 165 meq daily. He eats modest amounts of calcium and takes no supplements. He has reduced bone mineral density going back some time and takes Boniva a long acting bisphosphonate. He is clearly active despite only modest SS, his SS arises mainly from his high pH; why not stop the K citrate? Surely the high urine calcium is coming from his bones, and even the bisphosphonate cannot stop it. The best alternative is to let the pH fall if it will. Possibly all of this is from bone which provided alkali and calcium together. If the pH remains high and crystals still are forming, we may need a drug that forces bone to take up mineral. So the plan is to stop the K citrate and remeasure and then, if the pH remains high ask Dr. Murray Favus for advice on alternative bone directed drugs. As a matter of fact he should see Murray anyway because of his bones. There is a serious matter of cost because of his insurance situation but I have no alternative physicians in the city I know of as a substitute
6-1-2015 The Enterococcus Type D first showed up in December 2014 and have since been treated 4 times (Ampicillin, then Amoxicillin, the IV with Zosyn and Amoxicillin) most recently 14 days TID starting on 4-9-2015.
7-1-2015 Have discontinued the Gentamicin irrigations twice a day. Now intermittent cath every 8-10 days to keep vigilant on retention of urine. Residual amount is very low usually a few ml with an occasionally up to 30-50ml
7-15-2015 Today I saw Dr. Murray Favus as a referral from Dr. Coe at University of Chicago… Dr. Favus is an endocrinologist. He took my history, ordered a Dexa scan and that was done this morning. The scan revealed good and bad news and Dexa machine made lots of pretty color pictures, charts and whatnot. My spine is better than was the anticipation, though my hips are not. He places my risk of hip fracture very high at 80%. He has discontinued the Boniva and started me on Prolia by injection once every 6 months having had my initial injection today. The Prolia that he described as a large protein works by persuading the osteoclasts to quit gobbling my bone and a side effect of this treatment should be a reducing calcium in my urine that should help with reducing kidney stone formation.
8-5-2015 Dr. Fredriclk Coe’s follow-up: 60-year-old man return visit in follow-up. He had CaP stones, massive and accelerated as noted in my prior record. His labs showed a very high pH urine, hypercalciuria, was on K citrate and in retrospect believes there may be an association between the K Citrate and acceleration of stone formation. He takes CTD 50 mg daily and was hypercalciuric anyway without a high Na excretion. I was concerned about bone loss and Dr. Murray Favus saw him and put him on Prolea to halt further losses. Possibly some of the massive urine calcium loss is from bone, which is also a source of alkali. He is here today to review the new labs concerning stone risk. He notes that with cessation of the K Citrate he sees fewer tiny stones in his urine. Blood from 6/25/15 shows low creatinine paraplegia with reduced muscle mass; increased UA to 7.4 reduced Mg at 1.6 and high HCO3 low CL. Urine volume remains high at 3.9 liters, pH is lower but still high at 6.46, SS CaP is lower at 1.16 despite very high calcium of 340 with Na in a good range of 127. Prolia had not started by the time of the tests. Right now, his stone risk is better, and I am not unhappy. With the bone drug the urine calcium may well go down and we will be in better shape he went on the drug about 2 weeks ago. I would recheck in late fall at his convenience in hopes that the urine calcium will be down, and his stone risk be gone. He can schedule this with Kathleen as he wishes. \
Dr. Favus will be getting a serum calcium follow up in a few weeks. He remains on the CTD 50 mg daily. He is aware of our website I have pointed him to the article called Fluid Prescription which shows the benefits of fluids concerning supersaturation. Had kidney ultrasound, no hydronefrosis, two objects that might be stones were seen. Not a surprise…
8-19-2015 Labs (UA C&S) show all 3 bacteria with large counts Pseudomonas, Enterococcus Type D and Kelbsiella. Aside from Pseudomonas aeruginosa all remain sensitive to many different antibiotics. Though they all now appear to not being able to eradicate due to biofilms infected stone or whatnot. Meanwhile have a CT stone search on Monday. Expecting outcome to reveal a few stones though the mass stone production seems to have been stopped as I no longer see stone routinely in my urine. Biggest challenge right now is new bacteria and for such a simple beast I am afraid it’s winning. Time will tell. CT found 3 large stones.
12-3-2015 Perc-Neph was planned but canceled at last moment after consult with Milani and Coe. Reschedule pending result of 24-hour urine. Still waiting for that, CT last February reveal little has changed. No hydro noted, no obstruction. Received an order without background for 24-hour collection.
3-3-2016 Wednesday noticed more white floating crap in my urine with very mild odor. Thru night felt cold, not rigor took my temp 99.3 and I took some Tylenol. The same journey seen twice in the last 6 weeks, I expect it will worsen. Six weeks ago, taken in urine for UA and culture. The culture showed two bacteria and when I went into rigor and high fever was prescribed Cipro & Amoxicillin. After a few rocky days, I responded and finished the medicine. Four weeks later began to feel unwell again /took urine to the lab and when I had a high fever with the rigor I was prescribed Cipro. After a few rough days I become asymptomatic, around the 3rd or 4th day, rigor returned and after calling your office a second antibiotic was provided. The antibiotics were taken, and symptoms disappeared. Now just 8 or so days after finishing this course of antibiotics and symptoms are already returning. I am expecting chaos. I would like to take a urine sample to Adventist Lab partners first thing Friday morning and then wait for your directions.
3-4-2016 Friday began taking Tylenol around noon, followed up with Advil 3 hours later. I kept this program up throughout the day. The temperature was okay, didn’t sleep well.
3-5-2016 Saturday some blood was seen in urine. Stopped the Advil, blood in urine cleared up. Started taking Tylenol at 11 am, then 3 pm then 7, then 11 pm. didn’t sleep; around 1: 30 am rigor began, took two more Tylenol and around 3 am took my temperature and it was 101.7. The severity of the rigor had subsided followed with sweats. Grew a little concerned about blood pressure and wondering if sepsis with blood pressure collapse might be happening. Grateful that my blood pressure and the other interesting vitals were in my normal ranges so, at least, I got that going for me. Will be calling Milani’s on-call this morning to learn what interesting and exciting goat rodeo I’m invited to attend! As I think about all the misadventures since my brief visit with Dr. Schaefer (and I remind myself that he paid zero attention to the packet of records Dr. Milani had prepared for me), he can go bite me!
3-6-2016 Spoke with Dr. Will around 8:30am Sunday. Covered my fun history distant and recent). He said not of great concern about the little amount of blood seen on Saturday. We discussed options – prescribe medicine remain home, or hospital. I suggested I wanted to stay home if possible. He said okay, would review the recent history/labs and call in appropriate medicine to pharmacy. Picked up medicine (Cipro & Amox) them up around 10:15am and began taking. Mismanaged Tylenol and missed a dose and went in the extreme shiver mode around 8pm and had fun with that until 10pm or so, then more fun with sweats. This morning I have a normal temp. Vitals (blood pressure, pulse, etc.)) remain acceptable. Have I told you as a child I never liked merry-go-rounds, I like them even less (this one in particular) as an adult.
3-7-2016 Admitted to hospital, same old bug. Zosyn was selected. Discharge was a goat rodeo resulting from inattentive social worker that dropped ball (went MIA for 5 hours) on contacting Lexington home health nursing. Conclusion is they tried to keep me as inpatient, so their Adventist home health care agency could staff to accommodate if my discharge was delayed. Social worker provided me with false reason for the delay, claimed it was my insurance. Turned out Adventist health care at home did not have adequate staff to accommodate my home healthcare.
4-14-2016 Bi-lateral Percutaneous nephrolithotomy by Dr. Milani. Fully successful and according to Milani and KUB no remaining stones aside from a few that have dropped into the bladder. Dr. Dumitru (Infectious Disease Doctor) switched me from Zosyn to Ceftazidime because the minimum inhibitory concentrations (MIC) with Zosyn was increasing. Did have a few hives that popped up, treated with Hydrocortisone and Benadryl and finished the antibiotic without further problem, however a week later developed some hives on my elbows and right buttocks. After a few more days those symptoms disappeared as well. Internist had prescribed prednisone but by the time the prescription was available the hives had cleared up. Now about 50 days post operatively and doing okay.
2016 Epididymitis 2 ER visits, 2 PICC lines last one was Nov 18, 2016.
2016 Dr. Botsoe ordered Cologard test in lieu of colonoscopy due to the crazy 4-day hospitalization regime many years ago that was negative with no popups. Cologaurd was negative for cancer for whatever value this test provides.
2017 Recurrence of sepsis with pseudomonas and epididymitis, treated with IV Zosyn, and has occurred several with 3 or 4 ER trips with 3 hospitalizations… I think Dr. Milani has pretty much washed his hands of me and believes a diversion is the only way forward for me. Note Dr. Milani did not have the complete story of diversion, and he told me they left balder just rerouted the plumbing. Turns out to not be the case. Won’t consider intermediate steps like the vasectomy. Dr. Dumitru is suspicious the bugs are in my prostate as did Dr. Schaefer. PICC insert in right arm was more than normal difficulty and took two attempts – probably getting into trouble with PICC from too many 15-20 or so over 10 years. A urologist many years told me to eat potassium citrate that will make the stone disappear – don’t remember his name long time ago. No analysis of stones or routine when he made this claim. Others have told me if I get rid of the stones, the infections will stop. Dr. Milani was hot to trot on a diversion a few years using my appendix as the route for the urine to exit. He no longer speaks of this procedure, maybe it was called the Mitrofanoff procedure… And now were back to this diversion business and I am suspicious that it won’t alter my trajectory.
4-27-2017 Follow-up from hospital discharge with Dr. Botsoe, Long-standing discomfort with her covering several years ever since the fiasco where Dumitru advised no treatment and Botsoe intervened and with no uncertainty treated me with antibiotics. When it all blew up she chooses to recall the events completely different and puts the result on me for nagging her for antibiotics. I emphatically insist that did not happen and since then we don’t trust one another, and this leaves me searching for a new Internist. Further, don’t have confidence in her partners Meanwhile, my hypertension is building and Dr. Botsoe has upped the Atenolol from 25 mg once a day, two 25mg twice a day to 50mg once a day then to 50mg twice a day. BLOOD PRESURE is still variable with both in range reading and then higher 150/90 – 161/95 was the highest I have seen. This morning it was 151/64 and I had taken the 2nd atenolol around 2pm the previous day and with that had good control all yesterday afternoon and evening. So we have more work to do. Dr. Botsoe also announced at a visit a few months ago that she diagnosed me with Dysthymic disorder. I don’t believe she knows me anywhere well enough to make such a diagnosis.
5-9-2017 Was seen by Dr. Hairston (urologist) at Northwestern. Was there for video urodynamics. Test was canceled as Dr. H. did a cysto and a found a normal neurogenic bladder, however he found that I have a large divictuala of the urethra and believes that is likely the cause of my recent uptick in problems. The cure is a diversion with the total removal of bladder, prostate and related bits fashioning new exits from small intestine exiting through my abdominal wall. Lengthy conversation, he suggested foley as possible bridge to make me more stable while I am managing this decision. Order CT and will refer some of his patients that have had this surgery and will get me a consult with them. My fears are this will adversely impact quality of life and I’m not interested in life without quality and one of my major points of consideration is my independences and ability to self-care.
8-00-2017 Another infection and another PICC at Good Samaritan hospital.
8-30-2017 And the bacteria resistance profile suddenly changed for the worse.
Getting this new information was very unsettling and forced me to carefully consider my options. My conclusion I have no other chance aside from moving forward with the diversion surgery.
9-15-2017 Had another PICC placed at Good Samaritan started on Meropenem. Started using Good Samaritan Hospital exclusively for PICC because Adventist La Grange and Hinsdale were too slow or failed to respond in scheduling insertions.
9-29-2017 Had PowerPic central cath inserted, it outpatient surgery and the interventional radiologists at the hospital. I declined anesthesia.
9-30-2017 PICC was pulled and started using PowerPort clearview
10-02-2017 Percutaneous nephrolithotomy on left kidney at Northwestern with Dr. Nadler. First time I met him was just before the surgery and I saw him twice after that for about 1 minutes each time. One other revelation for the first time ever, there is risk of blindness from this type of surgery, a surgery that I have had several times, and this was the first time I had ever need advised about this risk I am believed to be stone free.
10-5-2017 A Bard PowersPort Implantable Port was inserted in my body on 9-29-2017. All events around that insertion were top notch and as of 10-5-2017 I have no discernable ill effects from the implementation. However, I have increasing confusion over what type of Powerport was implanted and the flushing schedule demanded when inactive. Perhaps it’s a documentation inadequacy or other labeling problem or perhaps a simple explanation is that I am an idiot. In any event, I am eager to follow the correct regime to keep the port operating and reducing the incidence of Sepsis. Here is an snip from the identification cards I was provided.
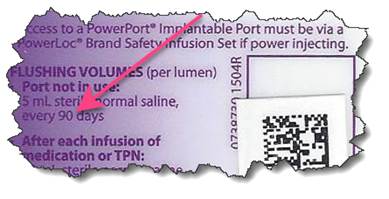 Figure 1. Snippet from the ID cards provided, full card reproduced below.
Figure 1. Snippet from the ID cards provided, full card reproduced below.
Note the word Groshong does not appear anywhere on my card. Equally important the flushing interval on these cards indicates flushing every 90 days when not active. Elsewhere in your information pack its instructs that inactive non-Groshong ports need to be flushed every 28 days and NOT 90 days as my card indicates. Calls to the hospital and to Bard provided no useful information and at one point I was quizzed why do I care. 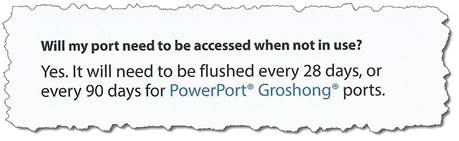 Figure 2. Snippet from the Bard pamphlet provided and reproduced in full below.
Figure 2. Snippet from the Bard pamphlet provided and reproduced in full below.
So the dichotomy is that I have a card advising me to have my port flushed every 90 days, yet all evidence suggests I have a non-Groshong port that requires flushing every 28 days. So my question is simple what type of port do I have and what is the right schedule. No rush as I have at least 28 days left…
10-15-2017 It’s now confirmed that I was supplied the wrong card and I need the flushing schedule for the non-Groshong port. Bard’s solution was to send me a blank card. Since the error according to the hospital was in manufacturing I wonder how many folks out there are running around with the wrong information…
12-5-2017 Assuming I stay healthy I will be admitted to Northwestern Memorial Hospital on December 5th, for the planned Radical Cystectomy and Ileal Conduit surgery to take place on December 7, 2017. I am apprehensive yet do not see any alternative that has an opportunity for a better outcome. Time will dispel any doubt and I’m hoping for a good outcome, so my journey might continue. This link is to patient guide outlining the procedure (cancer cause centric not my problem but it’s all the same) and the outcome. Doesn’t focus too much on the complications that range from death to additional surgery… https://goo.gl/RcX1CQ Doctors and Test Results: It is important to make sure that your bladder is emptying fully. This one issue probably has a direct link to my frequency of infection. Do not rely on the doctor to find this solution. In my case, my position (sitting versus laying prone), the type of catheter and how it is applied, all have a role.
Question the result of tests. If the doctors are not receptive to your questions, loose them sooner than later. You don’t need prima donnas; you need partners. For example, the Urodynamics test is designed to determine how fully your balder empties and what pressures are developed within your bladder. Too much pressure results in urine backing up into your kidneys. Over the years I have had several of these tests, all with normal values. The last test administered at Loyola was borderline. I believe those results are flawed because of several factors. I had an active UTI infection at the time of the test, and over my protests, Loyola required the test be done in a reclined position rather than sitting or prone, which is not a normal position for me. Based on the test results, which showed borderline pressure, they felt I needed to catheterize myself four-times a day. I did this for two weeks and most of the time there was no urine produced, which suggested a problem with their diagnosis. I observed that I emptied better in certain positions than in others. From that I found I could void fully (at least to the same level as was produced with a catheter) by changing my position. I confirmed this with self-catheterization. The Loyola doctors were not impressed with this information and told me to continue with their prescribed procedure. Do I need to state how I feel about these doctors’ abilities and manner? The moral of this story – don’t be complacent about doctors, reflux, bladder emptying, kidney stones or bacteria.
Pressure Sores
Butt: You and your butt are at risk, period. I had no problem with pressure sores during my first eight years of living in a wheelchair. However, on a trip to South America, I noticed a small spot of blood on the sheets. It’s really hard to see behind you so examining the bed sheets or your pants for any type of discharge, clear or bloody, is better than trying to use a mirror. I tried to ignore the problem, but it continued to get worse – much worse. I was then using the recommended wheelchair cushion, which was a thin 1.5 to 2″ heavy gel cushion. Whether my tissue wasn’t as resilient as I grew older or I got fatter or both, the gel cushion was not up to the task. I needed hospitalization (lengthy), plastic surgery and then, a number of years later, another surgery because the first patch failed. I now use a Roho air cushion exclusively. This cushion allows me to sit for as long as I like without any negative consequences.
Heels: I have also experienced breakdowns on the inside of my heels. I don’t know the direct cause, but I assume it was my shoes. I now use Reebok high-tops, which provide very good protection for my heels.& In addition, the shoe’s Velcro closures are easy to operate, and the shoes themselves are rigid to protect my feet when opening doors. Also I replace the standard shoelaces with elastic ones that do not need to be tied.
Penis: The last pressure problem I have encountered is on the base of my penis. This is caused by the external catheter. Care must be taken to make sure that no rolled up material from the catheter is left after the catheter is applied. The easiest way to accomplish this is to unroll the catheter just a little before applying. If you have some material left, carefully cut though the ring of material with a scissors – don’t leave it! Another technique I have used successfully when I notice redness is to place a Band-Aid over the area, and then apply the catheter over the Band-Aid. However, you must be extremely careful not to strangulate or otherwise impede the flow of urine with the Band-Aid. Even when not in strangulating, I think the Band-Aid may affect the flow so use with caution. Also, pay close attention to the adhesive liner on the catheter and move it when necessary by allowing more or less of the catheter to unroll before applying. I also use a skin protector called Skin-Prep, which I think provides better adhesion and protects the skin from breakdown. Skin-Prep also displaces any remaining moisture, allowing for faster application.
Hospitals: I can’t end this section without mentioning hospitals as they are important for my health. However, in my experience they are bit Jekyll and Hyde.
Lack of Accessibility: Adventist LaGrange Memorial Hospital has spent “zillions” of dollars building a new hospital to replace the decades old facility. Yet as recently as March 2008 when I was there for an x-ray, I found no accessible bathrooms serving that area of the hospital. At least the staff I asked were unaware of any; they directed first to one area and then to another. Neither bathroom was accessible and no signage directed me to an accessible bathroom. In my view this is inexcusable today.
Lack of Understanding: Another dichotomy is the ignorance of the nursing and patient care team regarding my independence and ability to provide my own care. Sometime during hospitalization, they invariably ask who takes care of me at home. When I tell them “I do” and that I drive, they don’t seem to comprehend. If that degree of ignorance exists in a setting where far more insight and empathy should be the norm, you can see why I believe the world remains a hostile place. Departments Not “In-Network”: Another major annoyance is that individual departments within community hospitals may be independently operated. They may not be “in-network” for your insurance though the hospital is “in-network.” This results in your paying more for services. You really have no say in this because you can’t control the specialties within the “in-network” hospital. This is an abusive practice. If hospitals outsource, they should insist on those providers accepting the same benefit levels as “in-network” providers and not bill the patient for the excess. This problem does not seem to exist in bigger hospitals, like Loyola or Northwestern.
Take Charge: You must always remember that this is your life that is on the line. I have been the victim of broken promises, bad charting, wrong diagnoses, lost paperwork and medical records, mistakes in billing and poor customer service. Today’s medical landscape involves numerous doctors, and shockingly the communication between them in my view is poor. I believe this is one aspect of a failure in the medical landscape. For example, when the urologists are done, they dump me to the infectious disease doctor and the on-going infection isn’t their concern anymore. This is a difficult problem. It takes tons of effort to get any cooperation and to convey all dimensions of your illness. Not every time and not always in the same facility but often enough to know that you must be your own best advocate. I accept that its a complicated environment, further complicated by government regulations, which I am not sure serve a real purpose. Often I get the sense that to a lot of the “players,” I am the least important component. The providers and insurance companies routinely seem to forget that I am indeed the “customer,” and the paying customer as well! To ensure that doctors orders are entered. you need to be aware of those orders. You need to make sure the orders are followed as written. You need to know your options and the risks. I can’t stress how important it is for you to be in charge of your welfare. Use any tools at your disposal to learn, learn, and LEARN more about your condition, various treatments and possible outcomes. It would be wrong to end this section with you thinking that I harbor only negative thoughts regarding providers and hospitals. That simply isn’t true, especially because I think I have an excellent group of talented doctors working for me. But unfortunately I think what has happened over time is that the greedy, the political, the lawyers and even bad patients with poor motivations have all discovered that the medical landscape is ripe to advance their own needs and agendas. I could pontificate more on this topic, but I am afraid it would neither be useful nor entertaining.